Telehealth Was Key During the Pandemic; Providers Want It To Stay Kansans Gain Greater Access to Care, Especially in Rural Areas
Published October 4th, 2022 at 6:00 AM
There’s a new mantra for medical care.
“Telehealth is here to stay,” providers and hospital administrators repeatedly said last week during a webinar presenting qualitative research on telehealth in Kansas.
The research, gathered by the United Methodist Health Ministry Fund and REACH Healthcare Foundation, found that 86% of Kansans support expanding or maintaining telehealth access after the pandemic ends.
Telehealth allows a patient to take an appointment from their home, via video or even telephone call. It was crucial during the pandemic as folks sought to minimize exposure to COVID-19. But in the past three years, providers and patients have found telehealth to be useful outside of times of medical crisis and a global pandemic.
Even as today’s public health emergencies fade, health care experts and providers are pushing for telehealth policies that will allow folks to continue accessing quality care.
Expanded Use
David Jordan, president and CEO of United Methodist Health Ministry Fund, said before the start of the pandemic, 11% of Americans had used telehealth.
The American Psychiatric Association found that number to be much higher, almost 40%, in May of 2021.
Jordan explained that telehealth could be used on a much larger scale due to policy changes implemented during public health emergencies.
These changes allowed patients and providers to take telehealth calls from home, on their own devices, sometimes over the phone (versus video call) and made sure providers were compensated at the same rates for in-person and telehealth appointments.
“This change made it very favorable to make it easier for both patients and providers to deliver, and access, health care via telehealth,” Jordan said.
Previous regulations around devices and location for telehealth calls stemmed from privacy concerns. As these loosened during the pandemic, Jordan said care was much more accessible and did not present significant privacy concerns as a result.
Telehealth expansion in Kansas was also possible because of temporary health orders which improved payment parity for the virtual appointments.
Providers were more likely to participate in telehealth services when they knew they’d be paid the same amount for virtual appointments as they would for in-person appointments.
Many providers were able to work telehealth appointments into their daily schedules, so Kansans were able to see their primary care doctors, psychiatrists and other local providers in person, or online.
Jordan said research around telehealth practices will be important as public health emergencies expire and organizations like his advocate for telehealth policies that will continue to facilitate the level of care seen in past years.
Rural Significance
Jennifer Findley, vice president of education and special projects with the Kansas Hospital Association, explained that telehealth care helps rural communities on several levels.
“Depending upon where you live, the access that you have to certain kinds of care can be limited,” Findley said.
Of the 105 counties in Kansas, 10 are without a community hospital, and 78 counties have only one community hospital, according to the Kansas Hospital Association.
Health care and travel went hand-in-hand for folks in these areas.
For example, someone living in a small, rural community, would probably have to drive several hours out of town for a heart surgeon, or an oncologist.
State of Health Care in Kansas
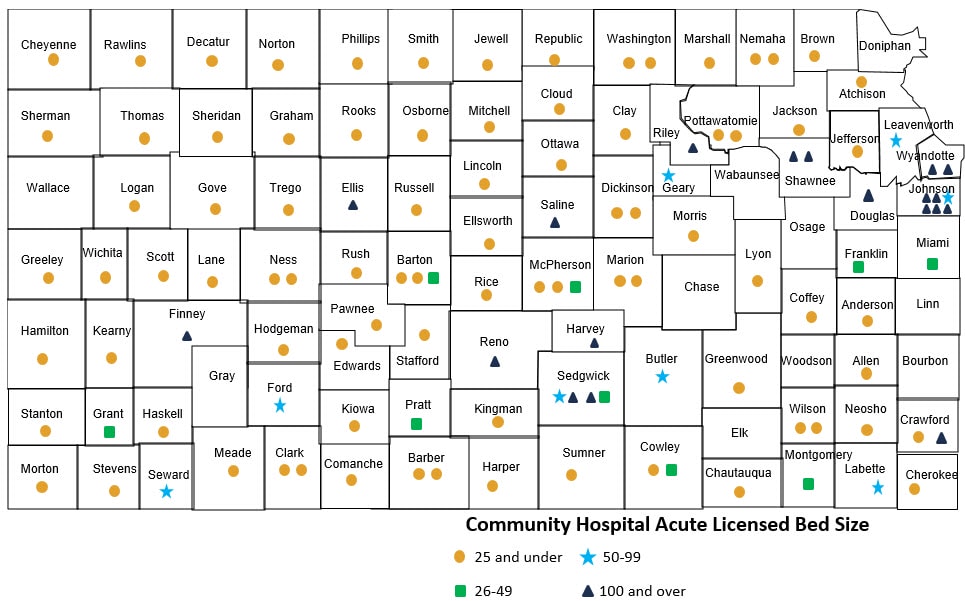
This presents an added burden on folks living in rural areas. Not only do they need to foot the bill for medical care, but also that of travel, more time off of work, a meal out of town or maybe even a hotel room for the night.
“Telemedicine helps equalize that access, it gives you the same access that folks in larger urban areas have,” Findley said.
Using the heart surgeon example, someone from rural Kansas would likely still have to drive to Wichita or Topeka for the actual surgery, but could do some pre- and post-operation appointments from their homes, or local clinics, via telemedicine. One trip out of town is certainly easier than multiple.
Findley said not only is there a cost to the individual who is traveling out of town, but to the community as well. Often folks will end up doing their grocery shopping, or other services, when they go out of town for a doctor’s appointment, rather than continuing to spend more in their communities.
“Telemedicine, in a way, is an economic development tool for a local community too, it’s helping keep those services all in town,” she said.
Findley explained that rural hospitals also benefit from inpatient telemedicine care. In this situation, a physician or specialist would be able to offer assistance or a second opinion via video call.
She’s also heard from nurses across the state who say they wouldn’t consider working for a hospital that didn’t offer telemedicine support.
Eagle Telemedicine specializes in this type of telemedicine and provides acute and specialty care to hospitals across the country.
It recently launched a program, aimed at helping high-risk pregnancies, that provides maternal-fetal medicine specialists to rural areas via telemedicine.
Matthew Goggin, the senior vice president of marketing for the company, said telemedicine is the best way to meet the staffing shortages facing hospitals across the country.
Goggin said that in interviews he’s had with rural hospitals, regardless of specialty, recruitment is difficult.
“In order for hospitals to continue operating and to serve their communities properly, they’re going to have to have access from a telemedicine perspective,” Goggin said. “We don’t have enough physicians across any specialty to fulfill the needs of every single hospital when it comes to physical physicians. We have to address it from a virtual standpoint.”
With telemedicine, Goggin said there could be one specialist living in Atlanta, but serving 5-10 urban and rural areas via telemedicine.
Goggin said there aren’t enough doctors in the country to serve the population. The ratio between the two is “a big challenge” the country will have to face.
“That’s why (telemedicine) is so important across the board,” Goggin said. “This isn’t just an (maternal-fetal medicine) issue, it’s a health care issue.”

Michael Byman, the company’s vice president of business development, said telemedicine also helps to address some of the issues facing young medical school graduates as they enter the field.
Gone are the days, he said, of the old school physicians with a private practice with a “mission-driven mindset.”
“It takes two brand new physicians, or one and a half to be able to replace an old timer,” Byman said. “That mindset is different with the physicians that come out of school right now. It’s all about quality of life.”
Byman believes telemedicine is the only way to meet the needs of physicians who don’t want to spend every waking hour at the hospital, but want the freedom to stay home with their families and work from home.
Eagle Telemedicine has several physicians who retired from working in hospitals but will work part-time via telemedicine because it allows them to continue to help patients from their home offices.
“They love helping people,” Goggin said. “What they hate is the paperwork, and the politics of medicine.”
Keeping Telehealth Accessible
Every patient and situation is different, so the policy framework must remain flexible around telehealth. Jordan said this will ensure folks get the right type of care and physicians can facilitate it and get compensated evenly.
“What we heard is that patients and providers want the flexibility to continue to deliver care in the way that works best for patients,” Jordan said of the Health Fund’s research.
In addition to payment parity and flexibility around devices, Jordan said providers want policies that allow telehealth integration into their clinics, technical support and increased broadband access.
Many Kansas physicians have been able to see patients through telehealth services, but Findley explained that some insurance companies will only allow telemedicine with a company, or set of providers it has contracted with.
“They restrict who can provide that telemedicine and that’s not something that we think is in the best interest of the patient,” Findley said.

Patients tend to be more comfortable with the physicians they already know, plus it makes it easier to integrate the information gathered from a telehealth appointment. The information from that telehealth call will go right into the patient’s chart so future visits (online or in person) will have the updated information.
Advocating for telehealth will be important as legislatures return to session.
Jordan expects to see bills in Kansas about telephone-only telehealth calls, and broadband expansion. At the federal level, he said there is a possibility of extending the current flexible frameworks for another couple of years to allow more study around best practices for telehealth.
“We want to continue to maintain these flexibilities both at the state and federal level and build a system that works for patients and providers,” Jordan said.
This article has been updated from a previous version.
Cami Koons covers rural affairs for Kansas City PBS in cooperation with Report for America. The work of our Report for America corps members is made possible, in part, through the generous support of the Ewing Marion Kauffman Foundation.


