An Epidemic of Sleep Disorders: Here’s What KC Experts Suggest Rates of sleep disorders have nearly doubled, studies show
Published July 19th, 2022 at 6:00 AM
Above image credit: The American Psychological Association long called sleep disorders an "epidemic." COVID-19 made things worse. (Adobe)Tamicka Monson was 7 years old when she first noticed sleep problems.
Monson, now in her early 30s, is among nearly 70 million people nationwide with one or more sleep disorders. A few years ago, she was diagnosed with three.
Growing up, access to mental health and overall health resources was limited for Monson. She chalked it up to childhood trauma. Instead of childhood, her days were full of checklists.
Tend to her younger siblings, check. Go to school, check. Substitute for mom, check.
“When I got home from school, I would just take, like, ridiculously long naps,” Monson said. “It just got progressively worse.”

Fast-forward to early adulthood. Monson would either sleep in too late or nod off just about anywhere. In college, it came to a head when two of her younger siblings died. Her already irregular sleep schedule was interrupted by nightmares.
Life dragged on. She would nod off as soon as the TV was turned off. Road trips were no longer feasible, with once-easy 8-hour drives to Chicago now dangerous.
“I started to feel like I could barely make it to St. Louis without taking like, three roadside naps,” she said.
She needed help, and fast.
So she shuttled from one doctor to another to find answers. All she got were incomplete diagnoses and sleep medications that didn’t work all of the time.
Some physicians blamed poor sleep hygiene.
“As a Black woman, and also somebody who has a larger weight, I’ve always been shamed,” she said. “It’s a really dehumanizing experience to go into places and the first thing that (a doctor says) is not, ‘What’s happened?’ but it’s always, ‘You gotta be doing better.’”
Monson knew it was something else. She pushed back.
After years of struggling, she was diagnosed with insomnia, sleep apnea and narcolepsy.
Today, Monson is a licensed therapist and has worked in behavioral health for a few years. She draws links between her mental health issues to sleep irregularities.
She can’t help but dissect her own experience with sleep disorders and their effects on her mental health.
“It’s been a really big struggle,” she said. “There’s not a lot of awareness around (sleep disorders) …”
Sleep, by definition, is a “distinct neurophysiological state. Sleep serves a restorative function for the brain and body, and is an integral part of overall health and a source of physiological and psychological resilience.”
— Current Cardiovascular Risk Reports, National Library of Medicine
Poor Sleep = Disease
While studies on sleep health and inequities are rare, new research has emerged in the past decade or so, gaining momentum during the pandemic.
A growing number of clinical researchers, psychiatrists and physicians are focused on the widening health inequities likely tied to sleep health, according to the Sleep Foundation. Factors tied to sleep-related illness include discrimination, jobs, housing, money and stress, to name a few.
Each one of these factors was amplified by the COVID-19 pandemic.
A 2015 study found that sleep-related disorders, such as obstructive sleep apnea, are nearly two times as common in communities of color. The same survey also found Black, Native, Pacific Islander, Asian and Hispanic folks reported they routinely slept less than six to seven hours per night.
Poor sleep increases the risk of chronic diseases, such as obesity, heart disease, Type 2 diabetes, and problems with immune function, according to the Centers for Disease Control and Prevention and American Psychological Association.
“There’s no organ in the body that is not touched by lack of sleep,” said Dr. Abid Bhat, a sleep medicine specialist at Sweet Sleep Studio and a professor at the University of Missouri-Kansas City School of Medicine.
During his time studying pulmonology, he was drawn to sleep research. Much like a neural network, identifying sleep problems can help physicians diagnose a health issue more accurately.
Folks who live in rural areas also experience poor sleep schedules and quality sleep because of longer commute times, few health clinics or hospitals in their areas, higher rates of poverty and overall poorer health.
The same goes for people living in lower-income areas in more urban parts of the city.
However, diagnoses across these populations are often delayed. This exacerbates health inequities, according to a 2015 study in the Sleep Research Society’s official journal, SLEEP.
The American Psychological Association called “disrupted sleep” a hallmark of the pandemic.
Experts are connecting the dots between pandemic-spurred stressors and sleep issues they are seeing crop up. Large swaths of the population in every industry are being impacted, they say.

Rebecca Robillard, a professor and researcher at the Brain and Mind Institute at the University of Ottawa in Canada, has led such research. Robillard is also a trained psychologist so her work has focused on the links between sleep and mental health outcomes.
“Sleep is so cool. It’s really mysterious,” she said.
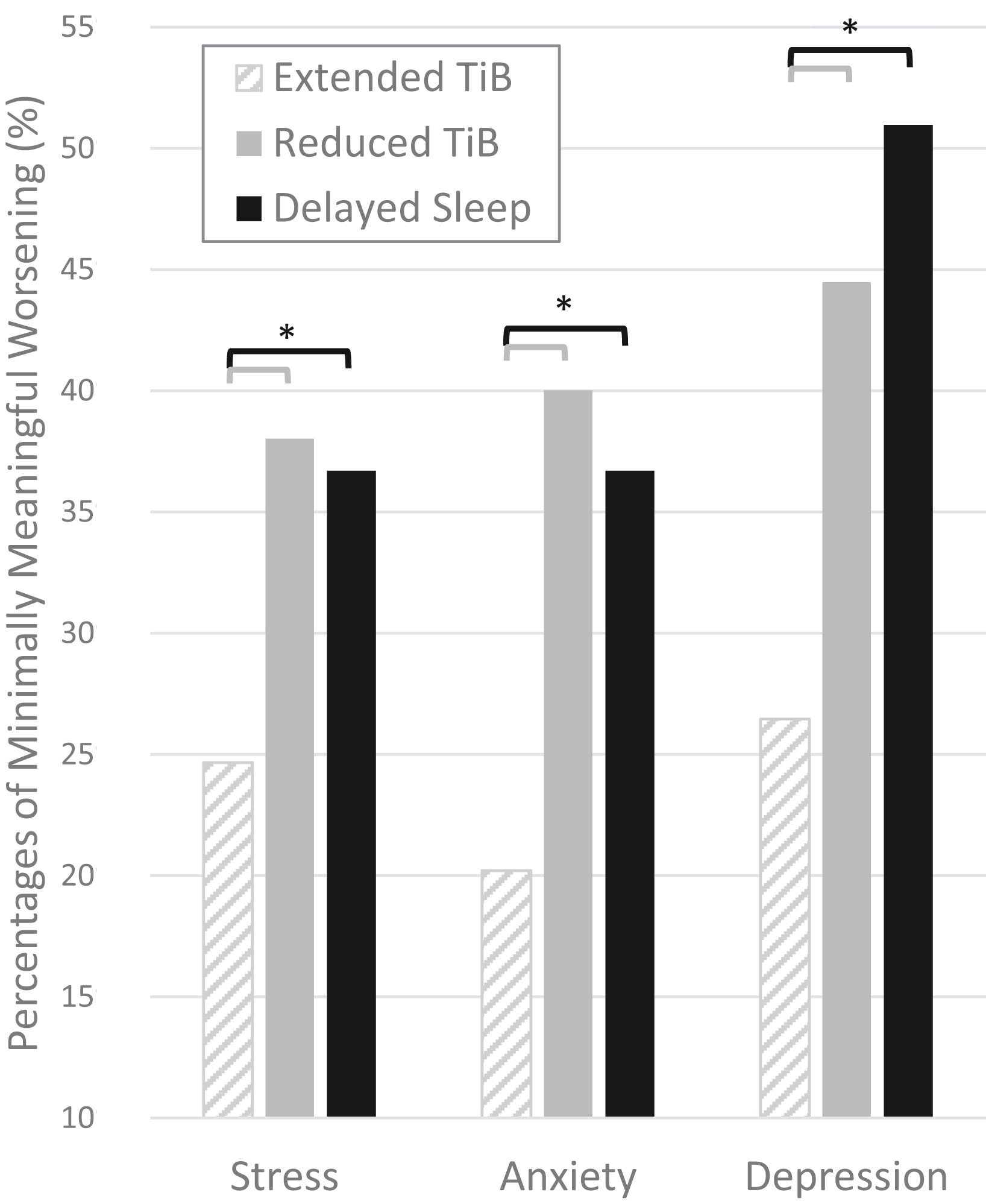
Her paper in 2021 showed high rates of anxiety and depression among those whose sleep patterns changed. That was true not only in Canada but also across the globe.
Robillard attended the World Sleep Congress meeting this year, and heard one by one as presenters from Italy, South America and Germany all reported similar trends.
Stressful life conditions placed undue pressure on folks, which spurred restlessness and exhaustion. Rates of anxiety, burnout and stress rose dramatically among health care and essential workers. The nature of their work exhausted them physically and mentally.
Workers like that were in a state of “hyper-arousal” — a condition linked to traumatic events preventing one’s ability to rest. This is known also as Post Traumatic Stress Disorder.
For those who worked from home, the lines separating home life from professional life were quickly blurred. Experts say healthy boundaries and sleep routines, also known as “sleep hygiene,” disintegrated.
“Sleep is actively involved in a lot of restorative function, both from a mental health and physical health perspective,” Robillard said. “By protecting our sleep, we’re equipping ourselves better to be able to face stressful situations and all the kinds of the challenges that we have to face during the daytime.”
Key Findings in Robillard’s Study:
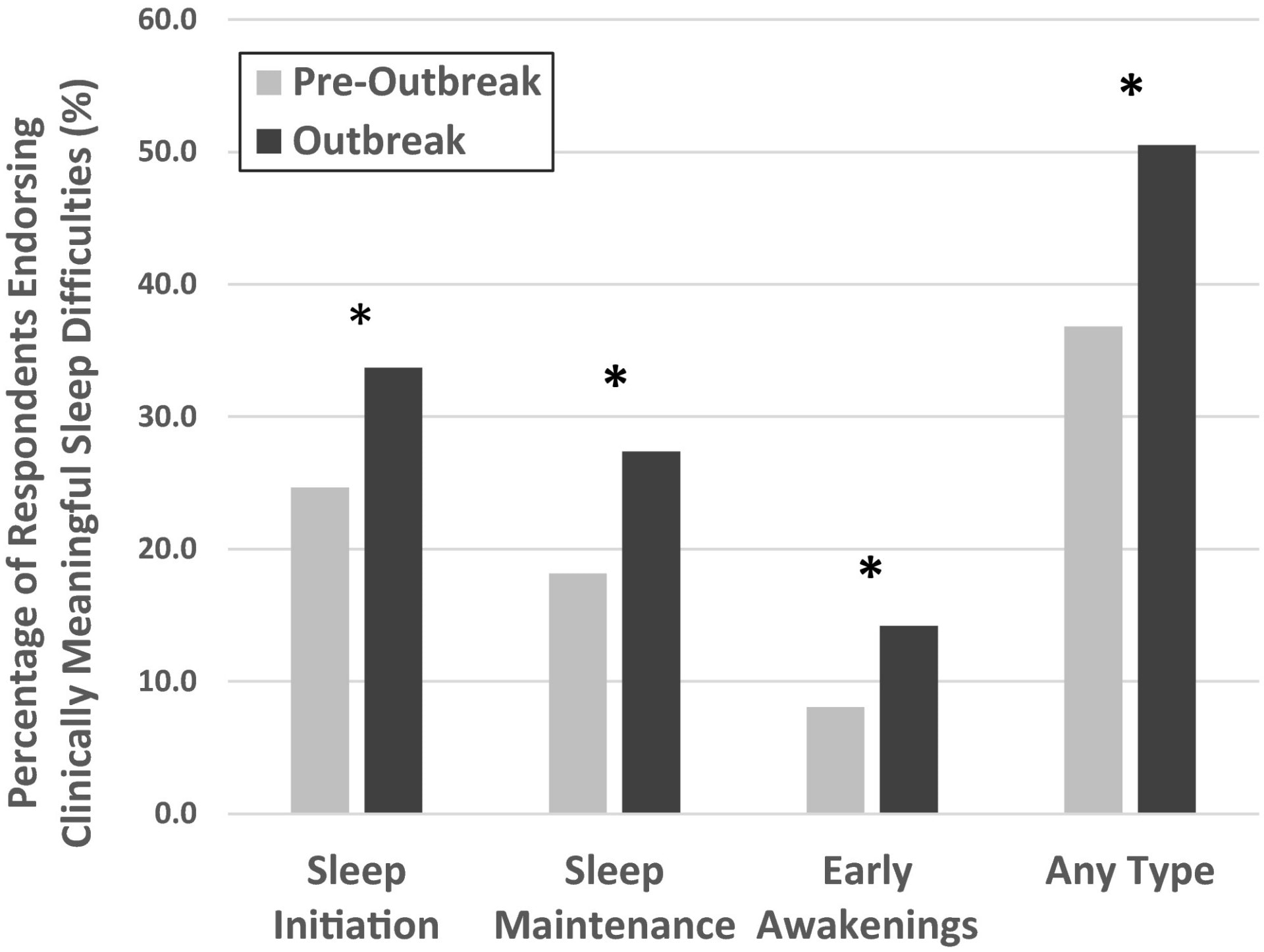
Slide 1: “TiB” means “time in bed.” Slide 2: Sleep patterns shifted during the outbreak when compared to pre-outbreak sleep patterns. (Robillard, “Profiles of Sleep Changes”)
Sleep issues also rose among children, Bhat said. In the past several months he has treated more children than ever before. National statistics mirror what he sees.
“The pooled prevalence of any sleep disturbance in children during the pandemic was 54%,” one 2021 study found.
During COVID-19 lockdowns, routines were disrupted and sleep quality dipped.
Psychologists and physicians attribute that to several things, such as the uncertainty surrounding illness, loved ones’ risk of getting the virus, work-life balance, child care, loss of employment and overall social isolation.
Rates of anxiety and depression have also skyrocketed during the pandemic, contributing to the disorders doctors have seen. Nielsen data showed that sales of sleep aids for pandemic stress-induced insomnia increased by 42%.
“Sleeping more or less than recommended — typically 7 to 9 hours a night — is a significant predictor of death by any cause,” according to the American Sleep Association.
Robillard’s research tracked just that, in addition to therapies and preventative measures to curb the effects of poor sleep.
A key part of her work has been on mood disorders, which can be regulated by establishing sleep routines and getting quality rest. Part of that, she explained, has to do with the biological clock and the way our bodies wind down. Heightened stressors have altered the way folks can relax, she explained.
Some ways are healthier than others, but experts have found success in a combination of treatments.
Both Bhat and Robillard support the use of Cognitive Behavioral Therapy Intervention (CBTI). CBTI could reduce prescription medication dependency and have longer-term benefits, Robillard said.
“This is a public health issue,” she added. “This should be part of our view of medical health as well.”
But most folks don’t know they may have a condition linked to poor rest or sleep disorder, Dr. Bhat said.
Before the pandemic surfaced, poor sleep was already an epidemic. Now the need for treatment is more dire.
Sleep Doctors’ Advice
Bhat put it like this: “Sleep is like hunger,” he explained, emphasizing how essential it is to overall wellness.
This is why too much and too little can tip the scale.
“If you eat food for lunch or dinner, you can’t have another dinner within an hour or two,” he added.
Therapists at the Sleep Studio in Kansas City work to retrain the brain and restructure a life around healthy sleep practices by using several different methods. Not only do patients come in for sleep studies, but they are also provided alternative therapies such as acupuncture and cognitive behavioral therapy.

Bhat said the goal is to identify the symptom and then help patients build better habits for the longer term.
“(Sleep) is not a switch, on-off,” he said.
For folks who’ve grown accustomed to sleeping in short spurts, for example, try to refrain from naps longer than 20 minutes. He also advises separating the wind-down process at night.
For example, for folks with anxiety about to-dos, find a time several hours before bed, and make a list of everything in the living room or a room that isn’t the bedroom. Often his patients have built habits that make their brains associate the bedroom with a stressor.
Re-conditioning the brain will take some effort and time.
“What we’re doing is we’re bringing down that old building. It’s gonna be a lot of mess. A lot of dust. When you take it out, then we can (build) the new building,” he added.
“So (in the) first week or two, you’ll find it even harder to go to sleep. You feel more tired because you’re restructuring your sleep.”
From a patient perspective, Monson said self-advocacy is key to getting to the bottom of any health issue.
She’s had to be outspoken in doctor’s offices. To avoid being blamed or dismissed by new physicians, she rattles off all diagnoses, medications and therapies she’s tried in the past.
In doing so, not only is she clearly outlining her health history, but she also is preventing spending her co-pay on repeat medical advice.
She’s already spent $14,000 in co-pays this year and a half.
“You have to push back against the system that tells you, ‘You don’t know your body more than I do,’” she said. “There are so many sleepy people.”
Monson also shared a few tips for folks who are seeking help for suspected sleep disorders:
“Get a physical. In one of my physicals, I realized that I don’t get enough sunlight, so that fosters depression, and also can mess up your circadian rhythm,” she said.
Next, she recommends the CBT-i App, which is for folks with insomnia who are in cognitive behavioral therapy and seek independent guidance.
“It makes sure you’re getting out of bed when you wake up and you can’t go back to sleep,” she added. “Rather than laying in bed and being stressed about being in bed, actually get up.”
Finally, she recommends a small activity. Take a walk around the block, even if it’s only five minutes. Or park further away to get the blood circulating. Baby steps.
Monson, for instance, hired a dietician and found activities that relaxed her mind.
“Those days, I will say, have helped me,” she said. “And I’m not like one who goes into the gym for two hours and like, shreds.”
Bhat concurred with this recommendation. He has advised meditative practices such as Tai Chi or getting a massage.
Ultimately, sleep experts’ hope is for more people in the community to find support, in or outside clinics. For Monson, it’s about building community awareness and acknowledgment. Her final piece of advice is, “You’re the expert in your life.”
Vicky Diaz-Camacho covers community affairs for Kansas City PBS.